BRAIN ABSCESS IN A PATIENT DUE TO Cladophialophora (Xylohypha) bantiana
E.R.Silveira1, M.A. Resende2, V.S.Mariano1, W.A.Coura1, L.D.Alkmim1,L.B.Vianna, C.E.Starling1, G.G.Cruz1, L.H.A.Benício1, A.M.Paula1, J.A.Gomes1, G.D.Santos1, M.A.M.Macedo1, R.E.Salum1, M. Gontijo2, A.L. Rabello3 and R.B. Caligiorne2,3
1Departments of Nephrology, Clinical Pathology, and Infectology, Hospital Vera Cruz
2Department of Microbiology, Federal University of Minas Gerais
3Centro de Pesquisas René Rachou, FIOCRUZ
INTRODUCTION
Infection diseases remain as the principal cause of morbidity and mortality in allotransplantation as a result of heavy immunosupression (1,2). Cerebral phaeohyphomycosis have been frequently described in organ transplant recipients (3,4,5). Phaeohyphomycosis is an umbrella term proposed by Ajello (6) to describe a broad range of primary and opportunistic mycosis, which present melanized yeasts or hifomycetes in host tissue. According its anatomic localization, the phaeohyphomycosis have been described as subcutaneal, corneal or systemic. The cerebral phaeohyphomycosis is the predominant systemic form (7,8). The Cladophialophora (Xylohypha) bantiana species are among the principal etiologic agents of cerebral phaeohyphomycosis. This organism is characteristically neurotropic causing CNS (Central Nervous System) infections, mainly abscesses (9). According a recent review, the phaeohyphomycosis caused by C. bantiana is wide distributed on the world and 75% of the available cases occurred on males but at all ages (10).
The diagnosis of cerebral phaeohyphomycosys is based on histological features of the biopsy. The fragments of the biopsy are also cultivated at 25?C on Sabouraud Dextrose medium in the presence of cicloheximide and cloramphenicol. The growth of dark-green colonies, together with microscopic and molecular characteristics of the agent, is factors for species identification. The prognosis is generally poor despite of therapy (4,11).
We report a case of a 61-years-old black man, who presented a cerebral phaeohyphomycosis after four years of a well-succeeded renal transplant. The causal agent was isolated and identified as Cladophialophora (Xylohypha) bantiana. The strain was deposited on CBS (Centraalbureau voor Schimmelcultures/ PO Box 85167, 3508 AD Utrecht, Netherlands) with number code (CBS 102586). The sequences of the ITS (Internal Transcribed Sequences) domains of the ribosomal DNA were performed for the molecular characterization of the strain.
CASE REPORT
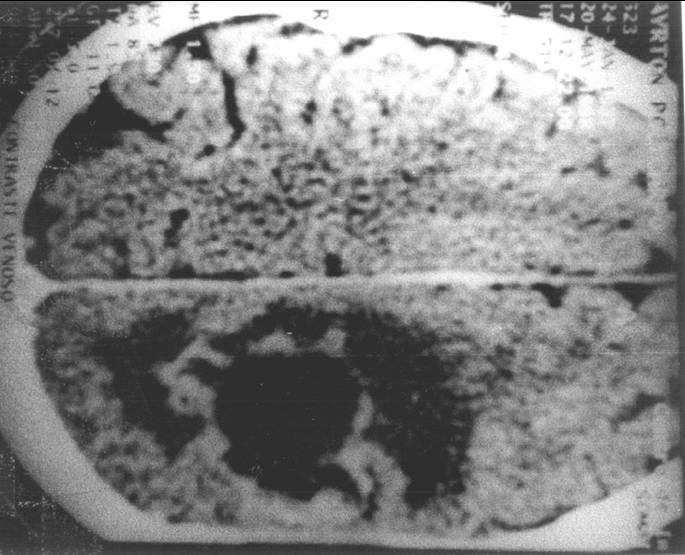
The patient was a 61-year-old black man, who was admitted to the Infectology unit of Hospital Vera Cruz in Belo Horizonte, Brazil, on January 1st, 1991, with heavy hematuria due to polycystic renal disease. He underwent unilateral nephrectomy of the bleeding kidney. Histopathological examination of the kidney revealed the presence of adenocarcinoma. After ruling out the presence of metastasis, it was decided not to treat the neoplasia. He was initiated on dialysis on January 22nd, 1991. On December 28th, 1993, the patient underwent a cadaveric kidney transplant. He had a primary non-functioning kidney graft and on day 7 he was treated for a possible acute rejection diagnosed by scintilography, receiving three 500mg pulses followed by four 250mg pulses of methylprednisolone. Urinary output gradually increased and the immunosuppression that followed was as usual in our service: Triple therapy with cyclosporine, azathioprine and prednisone. On June 6th, 1994, he underwent nephrectomy of the remaining kidney as a precaution measure. He never received mono or polyclonal antibodies. He was doing well until October 1997, when he started feeling numbness and pain in the right arm, which was thought to be, caused by the still functioning anteriovenous fistulae. However, after fistulae removal the pain remained and a right arm weakness appeared with slow progression. In the beginning of April 1998, he developed right hemiparesy. He was normotensive with no papiledema. He was admitted to the hospital and a CT scan showed an expansive lesion in the left parieto-temporal region of the brain (fig.1). On April 22nd, 1998, the patient underwent surgery with resection of a brown colored, encapsulated brain abscess. The histopathological examination of the tumoral mass revealed the presence of brown colored hyphae indicating the presence of a dematiaceous fungus (Fig.2). The examination of the material in potassium hydroxide revealed pigmented fungal hyphae. Culture of tumoral mass on Sabouraud dextrose agar in the presence of chloramphenicol resulted in the growth of dark-green colonies at 28?C in two weeks (Fig.3). The isolated fungus was able to grow at 40?C. Microcultures on Corn Meal Agar at 28?C for 30 days revealed long, flexuous chains of spores. The fungus was identified as Cladophialophora (Xylohypha) bantiana (fig.4). The patient became hemiplegic after surgery and was started on fluconazol 400mg/day and dexametazone for cerebral edema. Azothiaprine was removed and the dose of cyclosporine was reduced do 2mg/Kg of body weight. He became stable maintaining the neurological deficits. The CT scan was repeated on May 6th, 1998, revealing remarkable improvement on the cerebral lesion. He was discharged on May 11th, 1998 using fluconazol as a unique therapy for the abscess. On May 20st, 1998, he was readmitted to the hospital presenting weakness, fever and mental confusion. At that time blood chemistry was quite acceptable with urea of 61mg/dl and creatinine of 1.0mg/dl. He was quite anemic with Hemoglobin of 9.3g/dl and White Blood Cells (WBC) of 9600 cells/ml with no deviation. The CT scan was repeated and showed recurrence of the brain abscess. He was submitted to another brain surgery for removal of the abscess. On May 23rd, 1998 he was started on Amphotericin-B, 50mg/day in addition to Fluconazol. On May 31st, patient got worse, with fever and abdominal pain. He was normotensive and the blood chemistry was unremarkable showing normal renal function. However he presented with an elevated leukocyte count (16500/ml) with an important deviation (B=6%, S=81%, L=13%). Blood cultures were positive for bacteria Escherichia coli. The patient was started on ceftriaxone, 1g bid, but developed a septic shock and died on June 3rd, 1998. No autopsy was performed.
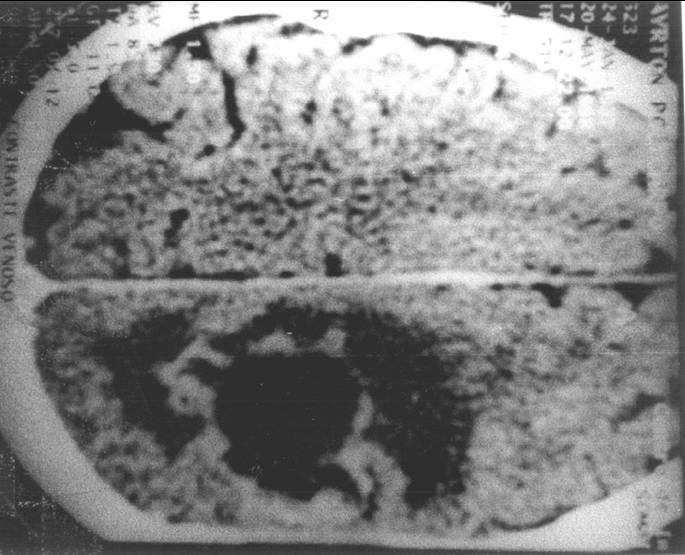
Fig. 1 - Computerized Tomography scan showing an expansive lesion in the left parieto-temporal region of the brain.

Fig. 3 - Culture of tumoral mass on Sabouraud dextrose agar in the presence of chloramphenicol resulted in the growth of dark-green colonies at 28?C in two weeks
DISCUSSION
The treatment of the phaeohyphomycosis has been unsuccessful in most cases, due to cellular immune deficiencies, diagnostic delays and sometimes the presence of multiple brain abscesses that turns difficult the surgical approach. However, some publications have reported a successful treatment in immunocompetent (12,13) and in immunocompromised patients (14). Our experience in treating the patient with fluconazol, without association with another drug, had initial good results. However, due to poor recovery of the patient, the recurrence of infection was almost immediate with the need of a new surgical intervention. The addition of Amphotericin-B to the treatment could not be evaluated since the patient became septic and died in a short period. The data available in the literature (5, 15,16,17) suggest that this type of infection must be aggressively treated with surgical excision (when possible) followed by antifungal chemotherapy using the drugs Amphotericin-B, 5-Flucytosine, Itraconazol or Fluconazol, alone or in association.
REFERENCES
1. ARUNKUMAR ML, RAJSHEKHAR V, CHANDY MJ, THOMAS PP, JACOB CK. Management and outcome of brain abscess in renal transplant recipients. Postgrad. Med J 2000: 894: 207-211.
2. SINGH N, HUSAIN S. Infections of the central nervous system in transplant recipients. Transplant Infectious Disease 2000: 2: 101-111.
3. MESA A, HENAO J, GIL M, DURNAGO G. Phaeohyphomycosis in kidney transplant patients. Clin. Transp 1999: 13: 273-276.
4. SARTORIS KE, BAILLIE GM, TIERNAN R, RAJAGOPALAN, PR. Phaeohyphomycosis from Exophiala jeanselmei with concomitant Nocardia asteroides infection in a renal transplant recipient: case report and review of the literature. Pharmacotherapy
1999:19: 995-1001.
5. SALAMA AD, ROGERS T, LORD GM, LECHLER RI, MASON PD. Multiple Cladosporium Brain Abscesses in a renal transplant patient. Transplantation 1997: 63: 160-162.
6. AJELLO L, GEORG LK, STEIGBIGEL RT, WANG CJ. A case of phaeohyphomycosis caused by a new specie of Phialophora. Mycologia 1974: 66:490-498.
7. McGINNIS MR, HILL C. Chromoblastomycosis and Phaeohyphomycosis: New Concepts, Diagnosis and Mycology. J. Am. Acad. Dermatol 1983: 8:1-16.
8. RIPPON JW. Phaeohyphomycosis. In: Medical Mycology. The pathogenic fungi and the pathogenic actinomycetes. 3rd ed. Philadelphia, W. B. Saunders Co., p.297-324, 1988.
9. DIXON DM, MERZ WG, ELLIOT HL, MACLEAY S. Experimental central nervous system phaeohyphomycosis following intranasal inoculation of Xylohypha bantiana in cortisone-treated mice. Mycopathologia 1987: 100: 145-153.
10. HORRÉ R, HOOG, SG. Primary cerebral infections by melanized fungi: a review. Studies in Mycology 1999: 43: 176-193.
11. MASINI T, RIVIERA L, CAPRICCI E and ARIENTA C. Cerebral phaeohyphomycosis. Clin. Neuropathol 1985: 4: 246-249.
12. UMABALA P, LAKSHMI V, MURTHY AR, PRASAD VS, SUNDARAM C, BEGUIN H. Isolation of a Nodulisporium species from a case of cerebral phaeohyphomycosis. J. Clin. Microbiol 2001: 39:4213-4218.
13. LIRNG JF, TIEN RD, OSUMI AK, MADDEN JF, MCLENDON RP, SEXTON D. Cerebral phaeohyphomycosis complicated with brain abscess: a case report. Zhonghua Yi Xue Za Zhi (Taipei) 1995: 55:491-495.
14. OSIYEMI OO, DOWDY LM, MALLON SM, CLEARY T. Cerebral phaeohyphomycosis due to a novel species: report of a case and review of the literature. Transplantation 2001: 71:1343-1346.
15. SEAWORTH BJ, KWON-CHUNG KJ, HAMILTON JD, PERFECT JR. Brain abscess caused by a variety of Cladosporium trichoides. Am J Clin Pathol 1983: 79: 747-752.
16. PALAOGLU S, SAV A, BASAK T, YALCINLAR Y, SHEITHAUER BW. Cerebral Phaeohyphomycosis. Neurosurgery 1993: 33: 894-897.
17. SUTTON DA, SLIFKIN M, YAKULIS R, RINALD MG. U.S. case report of cerebral phaeohyphomycosis caused by Ramichloridium obovoideum (R. mackenziei): Criteria for identification, terapy, and review of other know dematiaceous neurotropic taxa.
J Clin Microbiol 1998: 36:708-715.